Vagus Nerve Stimulation (Epilepsy)
Vagus Nerve Stimulation for Epilepsy
There are a variety of reasons to use Vagus Nerve Stimulation (VNS) to treat epilepsy. These include the potential for better brain function and the possibility of reduced seizure frequency. Patients who are refractory to other treatment options, such as medications and neurosurgery, may be candidates for this procedure. Its primary benefit is its ability to cure focal epilepsy and prevent seizures.

The main goal of VNS therapy is to stimulate the vagus nerve by delivering stimulation at specific intervals. The total percentage of time that VNS is on and off is known as its duty cycle. A typical stimulation on-time of thirty seconds and a five-minute off-time is 10%. Some patients achieve benefits from this regimen even at this low duty cycle. However, increasing the duty cycle may increase the benefits of the therapy. To do so, the patient must decrease the length of time that the VNS is off. For example, a 16-hour duty cycle would be equivalent to a 10 percent duty-cycle.
The risks and side effects of VNS are minimal. It is generally safe, but there are a number of complications associated with the procedure. Coughing, hoarseness, dyspnea, infection, and lower facial muscle paresis are possible side effects. During the procedure, the device should be inserted through a small neck cut. The electrical current is placed on the device, which acts as an electrode and controls the heart rate.
The output current of magnet mode is 0.25 mA higher than the output current of normal mode. The increased stimulation intensity may result in minimal side effects, including changes in the voice and a change in speech. If you are experiencing seizures, the next step is the higher setting. The doctor should monitor your progress closely. Your doctor should be able to adjust the dose accordingly to your symptoms. If the procedure is not successful, the doctor may recommend another treatment method.
This treatment is extremely effective. It has been used for over 20 years. It is FDA-approved in 1997, and has been implanted in over 100,000 patients, including children. Although VNS is not a cure for epilepsy, it can help control certain types of seizures, including partial seizures. It is not for everyone. The procedure may not be the right choice for everyone. There are several risks, and VNS is not the right choice for every patient. If you have a medical condition, you should talk with your doctor before undergoing this treatment.
The main benefit of this therapy is the increased ability to control seizures. However, there are several side effects associated with this treatment. The side effects of VNS include hoarseness, hives, and infection. If you experience a high-pitched voice, you may experience a coughing spell. Nevertheless, the surgery can be very beneficial for people with epilepsy. While the risks are low, it can help you avoid dangerous side effects caused by the medication.
While there are a variety of risks associated with this therapy, it is considered a safe treatment. The device is FDA-approved, and it has been implanted in over 100,000 children and adults with seizures. In many cases, VNS reduces the frequency of seizures and improves quality of life. Additionally, VNS can reduce the risk of recurrent seizure attacks. Moreover, it can help you recover from any ailment.
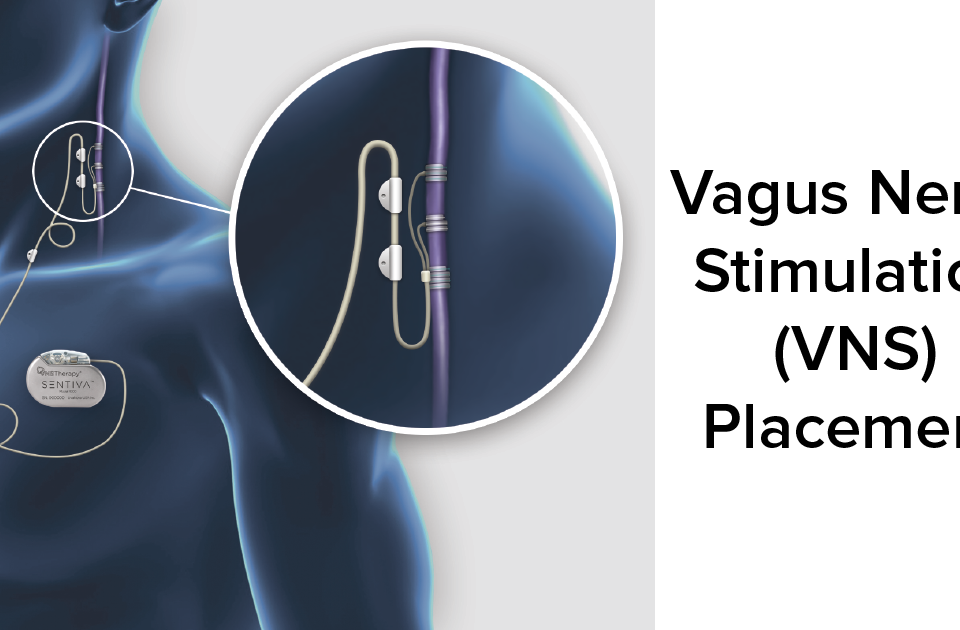
The procedure is usually done under general anesthesia. The VNS device is placed under the upper chest skin. A wire is connected to the electrode that is attached to the vagus nerve. A small incision in the neck is required to access the vagus nerve. The device will send tiny electrical signals to the brain to control seizures. The timing and frequency of the stimulation can be adjusted to suit the patient’s needs.
Although the VNS procedure is a safe and effective way to treat epilepsy, some risks are associated with it. There are risks associated with the surgery, which include coughing, hoarseness, and dyspnea. While the risks are minimal, the surgery can cause infections and lead fractures. The lead used to connect the VNS device to the patient is also connected to an electrode that is placed on the vagus nerve.